Today we’d like to introduce you to Shoshana Hallowell.
Hi Shoshana, so excited to have you with us today. What can you tell us about your story?
Cancer has always been a part of my life. As a General Surgeon, I treat cancer patients daily. Some days I get to tell them their cancer is gone and other days I must tell them it has recurred. My connection with cancer become much more intimate once I was diagnosed at 37 years of age.
I was the typical busy physician that put more time into patient care then looking after myself and ignored a lump that I felt in my breast for a few months. Once I finally had my imaging done and reviewed it myself, I knew immediately I did exactly what I tell my patients not to do: I delayed my own health care.
I had my biopsy done two days after my imaging and continued along with my busy schedule. Three days later in the middle of operating, I got a call with the phrase I’ve heard many times but the meaning now changed MY world forever: “Dr. Hallowell the biopsy came back positive for cancer.”
As a Surgeon, I chose the most aggressive surgical management and underwent a bilateral mastectomy with delayed reconstruction in 2020-2021. While my treatment is still a long road, with five years of anti-hormone therapy, I am grateful I was able to avoid some of the more aggressive treatment regimens that other patients must endure.
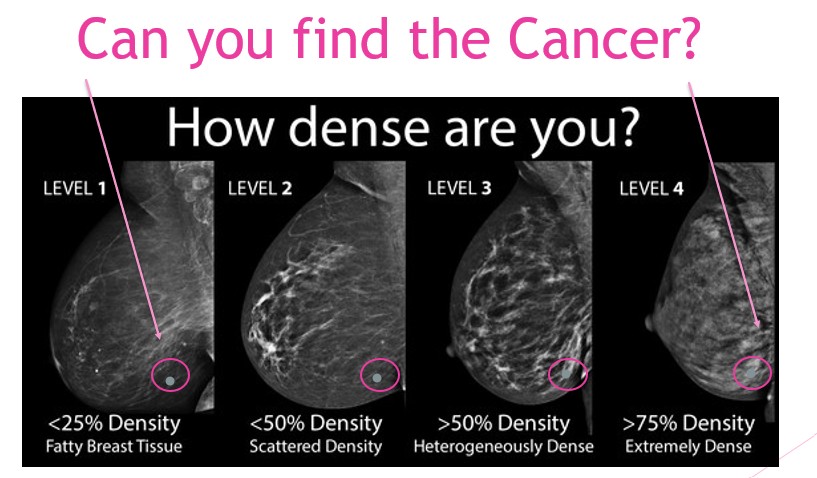
After my diagnosis, I encouraged my sisters and mother to get additional screening imaging as they were now high-risk patients due to me – their now cancer-affected first-degree relative. I insisted my sister inform her PCP of her elevated risk factors for breast cancer and that she needed to undergo a Breast MRI for screening. Her PCP recommended they wait 6 months to get the imaging as she just had a “normal” mammogram. However, what my sister was not informed about was that she did not just have a normal mammogram. She had a mammogram that indicated she had dense breasts. Mammograms miss a cancer diagnosis 40% of time in women with dense breast tissue. Therefore, it was indicated even without the family history that my sister undergo additional imaging for breast cancer screening. Six months later my sister’s MRI was finally done and she was diagnosed with a 2.3 cm triple-negative breast cancer. I immediately asked to see my sister’s mammogram reports from years prior. Her reports read that she had dense breast tissue for the last four years. She should have had that MRI four years ago! If she did, her diagnosis would have been at an earlier stage and her treatment regimen would have been much less aggressive. I could not believe this was happening.
After this finding, my family and I decided my mother needed to get imaging as well. My mother was 75 years old at the time and her last mammogram was two years prior. According to the to the US Preventative Service Task Force, mammography in woman over the age of 75 is not indicated. The American Cancer Society recommendations for screening in elderly women indicate that if the woman has a life expectancy of > 10 years then imaging should be continued. My mother is a healthy, active 75-year-old woman that was not being screened appropriately by her PCP. How did I not know this was happening? We made an appointment for her to get a mammogram the next week and my mother was diagnosed with DCIS two weeks later.
I was astonished! Not only am I in the medical field, but I treat breast cancer and my own family members were not being screened appropriately for breast cancer. How did I not know they were not getting the appropriate care? I just assumed their physicians were taking care of them. I assumed their risk factors were being evaluated. This was not the case and due to this my sister and mother suffered a delay in diagnosis. If this is happening to people with medical knowledge and medical advocates that even bring the information to their physician about the additional screening needs and are still denied proper care then can you imaging how many other women are being affected. I can tell you – it’s about 40% of all women. 40% of women have dense breast tissue and require this additional imaging. In addition, our elderly population is growing and living much longer and healthier lives. By no means should their screening be cut off due to age. Cancer survival depends on the stage at diagnosis therefore screening is essential.
95% of women do not know if they have dense breast tissue or not. In addition, 90% of women are not aware that dense breast tissue increase your risk of breast cancer by 4-6-fold. Although this knowledge was known in the medical community its translation to the public and patient care is still significantly delayed. It was not until 2009 when Nancy Capello championed the first in the nation breast density information law in the state of Connecticut. As of 2019 Federal legislation has made density reporting now standard of care in 50 states. However, this is still not always enforced.
In addition, screening guidelines for women with dense breasts have not been updated by the American Cancer Society, National Comprehensive Cancer Network, US Preventative Service Task Force, American College of Obstetrics & Gynecology, and the Academy of Family Physicians since 2015. Since that time there has been data providing evidence that ultrasound, MBI, and MRI find significantly more cancers than mammography alone in women with dense breasts, and are able to diagnose those cancers at an earlier age.
I have made it my promise, not only my sister and mother but to all women that I will do what it takes to make sure this does not continue to happen to women. Women need to be notified of their density and its associated risk, their physicians need to order the appropriate screening modalities indicated for their breast tissue, insurance companies need to provide coverage for these additional screenings and their cancer diagnoses need to be caught as early as possible to ensure their survival.
That is why I started the nonprofit organization Operation Breast Density. This organization is dedicated to breast density awareness. It will provide education to patients, health care providers, and physicians on appropriate screening modalities needed for this patient population. Advocate for updating screening guidelines to be put in place by national cancer organizations. Assist with standardized breast cancer risk assessment tools that take breast density into account as this is not the case in our current models. In addition, it will provide financial assistance to those in need who require supplemental screening for their dense breast tissue or higher risk factors.
Can you talk to us a bit about the challenges and lessons you’ve learned along the way? Looking back would you say it’s been easy or smooth in retrospect?
In regards to breast cancer treatment it was definitely not a smooth road which is common for most breast cancer patients. The treatment regimen is long and complex and there are bound to be hiccups. I have had a few complications with surgery. I had to go back to surgery due to an infection 2 months from my reconstruction surgery and now a year later I am facing having to undergo another surgery due to another complications. However, I am still thankful for that fact that my cancer was diagnosed early, and no matter what that has ensured a higher survival rate for me.
I also had to do IVF during the process to preserve embryos due to my age and that process was very difficult both mentally and physically.
Thanks for sharing that. So, maybe next you can tell us a bit more about your business?
The Mission of Operation Breast Density is to empower women with knowledge about their breast health to optimize and individualize their breast cancer screening. We aim to educate those on breast density and its associated risk for breast cancer development as well as promote awareness about the screening challenges of dense breast tissue. Our goals are to prevent missed or delayed cancer diagnoses in women to ultimately reduce the overall mortality of breast cancer patients.
The purpose of our organization is to educate, create access, and provide financial assistance to women enduring this healthcare disparity.
What quality or characteristic do you feel is most important to your success?
I feel a sense of gratitude is most important for my success. My focus on being thankful every day for the fact that I am still here to share my story and to make sure others do not have a delayed breast cancer diagnosis due to breast density gives me a sense of purpose and fulfillment. It helps me see the silver lining in the challenges I have had to face in that I can in turn help others.
Pricing:
- Average Cost of Breast MRI not covered by insurance $1, 000
- Average cost of bilateral ultrasounds not covered by insurance $250
- Average cost of treatment of patient diagnosed with stage 4 Breast Cancer $159,442
- Average cost of treatment of patient diagnosed with stage 1 breast cancer$ 84,487
Contact Info:
- Website: https://www.operationbreastdensity.org
- Instagram: https://www.instagram.com/operationbreastdensity/
- Facebook: https://www.facebook.com/OperationBreastDensity/
- Linkedin: https://www.linkedin.com/in/operation-breast-density-aa1499252/