Today we’d like to introduce you to Nisha McKenzie.
Hi Nisha, so excited to have you on the platform. So, before we get into questions about your work-life, maybe you can bring our readers up to speed on your story and how you got to where you are today?
When I was in 4th grade my great grandmother came to live with us so my mother could help with her many healthcare needs. She passed due to heart failure when I was in 7th grade. I remembering vowing through my tears that I was going to be a doctor (I had never heard of a PA at this point in my life!) so I could take care of people better.
Fast forward to college, I decided that earning a degree as a Physician Assistant was where I fit best – a place where I could practice medicine, without being so fully engulfed in medicine that I might be unable to have a family or be the parent I wanted to be. I loved this decision in every aspect. Even though 20+ years ago many still hadn’t heard of PAs and most of my patients thought I was a nurse or asked when I was going to finish school and be a doctor. It never bothered me though, I stayed comfortable and confident in who I was and what I was doing.
After finishing PA school, I worked in Family Medicine for 9 years, choosing this field because I loved taking care of families and observing how the inter-relational dynamics affected my patients. As I continued to listen to and to watch these dynamics, I began to recognize more and more how we can both positively and negatively affect the people in our lives, through small gestures, words, actions, and non-actions. I started to recognize how my female patients would carry the burden of the relationship differently than their male counterparts, who were also my patients. So many of my female patients would say, “clean the cobwebs out while you’re down there”, with a meek, nervous giggle afterward, while I performed their pap smears or their pelvic exams. I heard this as a cry for help, however, had minimal ability to respond other than an equally meek, nervous giggle.
I also began to recognize how women are left behind in medicine and in research, how the signs and symptoms we are taught to look for are the typical signs and symptoms we should see with the male version of the disease. Heart attacks, for example, often present as chest pain in males, but often present as back, shoulder, neck, stomach, or jaw pain in females.
I’ve seen many women come in with a fervent need to advocate for themselves based on previous experiences, and others who were unable to advocate for themselves also based on previous experiences. I’ve seen the women who do advocate for themselves be called bossy, hysterical, pushy, overdramatic, and overly emotional. The culmination of all of this and a female patient one day telling me she needed to improve her libido or her marriage was going to be ending, led me to a new resolve with my mission. I knew at that moment I needed to find answers for my patients, and I wouldn’t find them in the typical medical journals and conferences I was attending.
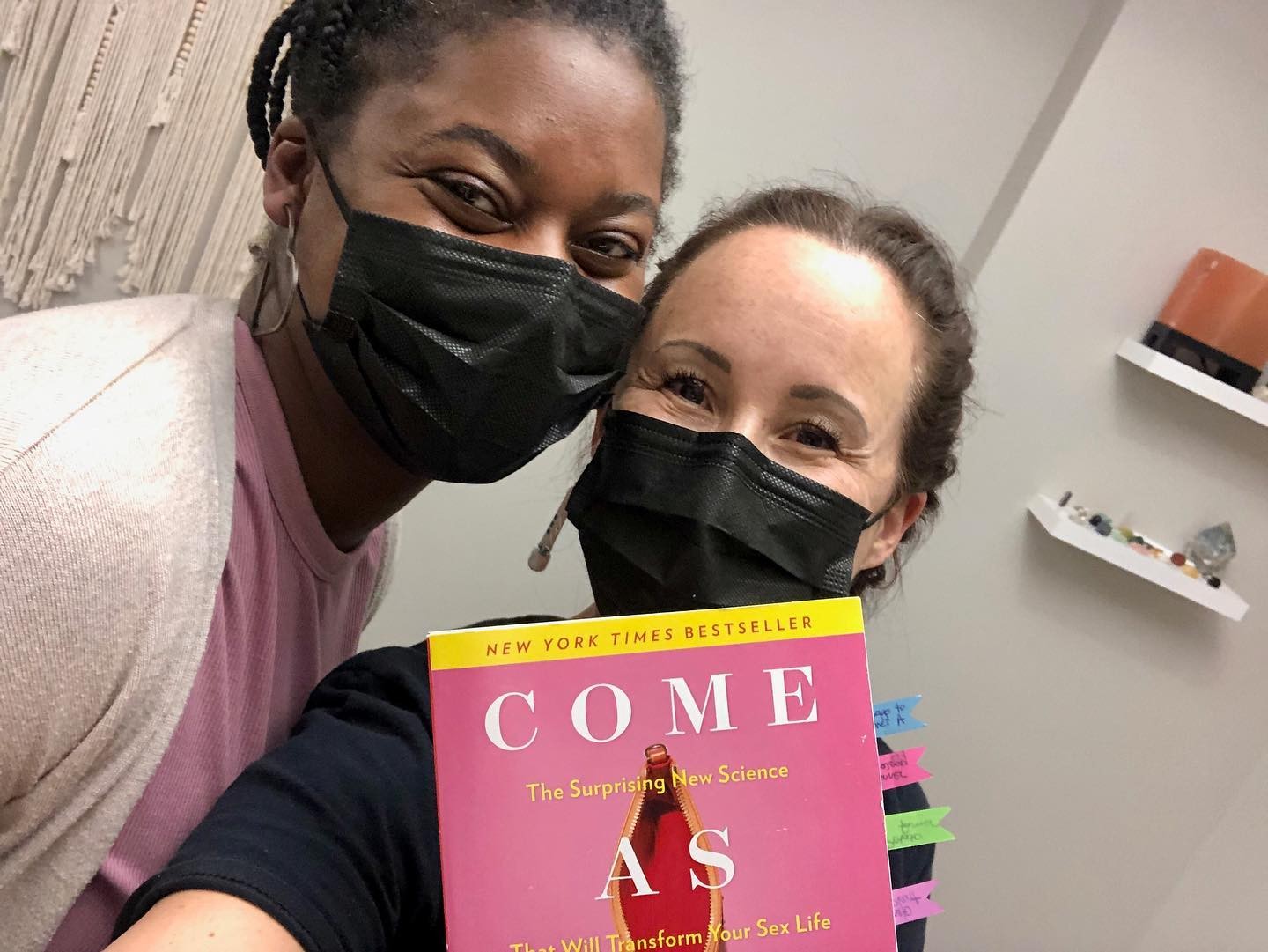
So, I sought out specific training for female sexual health. However, I knew that in order to truly focus on this study I would need to work within Women’s Health. There is just not the time in Family Medicine to focus so comprehensively on one (albeit very broad) topic. So, I made a move to work in an OB/GYN private practice after which time I attended conferences, subscribed to medical sexual health journals, and attended the University of Michigan’s Postgraduate Sexual Health Certificate Program to become a sexuality educator and counselor.
Along the way, I began to recognize that women were not the only people left behind in medicine. There are so many marginalized groups and individuals that are not only treated differently in medicine but also have different health outcomes. These disparities are often unnoticed by the very medical professionals acting on them thereby perpetuating the data clearly highlighting these health disparities.
And what started as a small fire, a drive to know more, to do better myself as a medical provider, so that I could better help my patients, turned into a burning passion to change the way medicine is delivered as a whole. The medical knowledge is not where we are falling short. We are falling short in the ability to effectively listen and then communicate what we know in a way that our patients can utilize in reality.
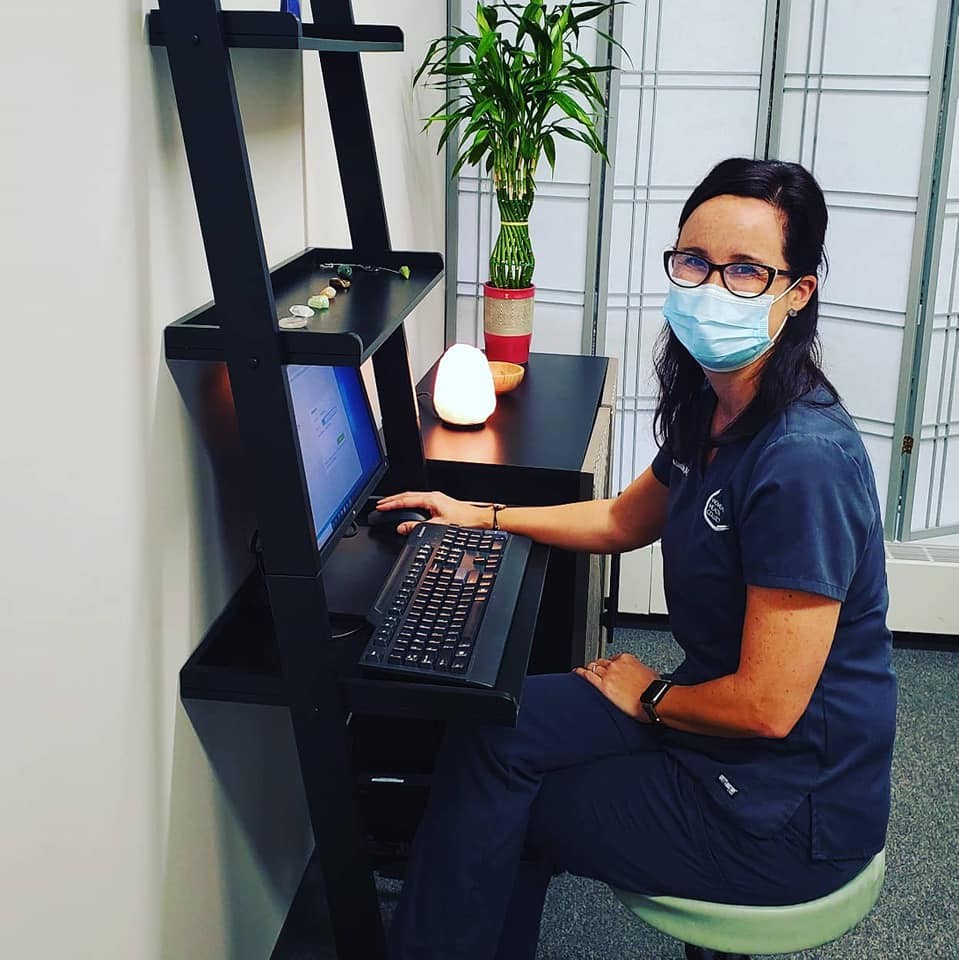
So, I decided to step way out of my box! I left a comfortable, safe job that I loved to start my own practice. A practice where I can train myself and staff in the empathy and diversity that I believe is required to effectively promote optimal overall health. A practice where I can listen to patients, spend the time I feel necessary with patients and consistently work to provide a safe space for them to tell me their stories.
I also wanted to create a practice that recognizes the myriad ways humans heal, some requiring western medicine, some eastern medicine, some more visits than expected, others fewer visits, some longer visits, and some less long. Some that require me to change my direction mid visit, because previous trauma might require a revision in our approach. And visits that allow patients to inform me what is standing in the way of their healing, including if that thing standing in the way is me, or my approach. I knew I needed to meet patients at their level, and that working together is the way we could best improve their health. I knew that the traditional proscriptive way medicine is delivered was not the way I could best help my patients heal.
And I knew I needed to increase access to care. So, although every one of my colleagues and mentors encouraged me to open a cash pay/concierge practice, this was not the place I needed to meet patients. Perhaps someday this will be the way most people access medical care, but today, most still need health insurance and can barely pay those premiums and copays, let alone additional medical memberships and visit fees. For now, a large part of my mission is to decrease barriers to accessing health care, and working within an insurance-paid model is part of how I need to do that.
I’m sure you wouldn’t say it’s been obstacle-free, but so far would you say the journey has been a fairly smooth road?
I’m pretty certain you’ll be hard-pressed to find a business owner who said it was truly a smooth road to opening! However, I’m also certain that overall, I can’t complain. I’ve had an incredible amount of support from my family, friends, as well as patients over the past 2 years since opening. I feel blessed beyond measure.
Some of the bigger roadblocks were, well, being a woman as well as being a PA (vs a physician). I had to very carefully and subtly educate quite a few resistant people or questioning professionals as I started to work with attorneys, accountants, banks, purchasing organizations, and insurances. Numerous times I was asked if I was sure I could even start my own business, called “hon” or “sweetie” by older men who clearly did not think I could do this (although admittedly I’m not exactly sure why they thought that since I never outright asked them). Multiple times people told me “I don’t think nurses (or MAs) can own a practice”. My response was always “I’m not certain if they can, but I’m a PA and I do know that I can”. Even then, I couldn’t find a healthcare attorney who knew how to set up a practice like I was, as there are no other prototypes like it, no precedent set. So, I ended up reading and learning the law, in all its fine print, and bringing it to attorneys to show them what I could do.
And of course, there was that little piece about opening a multi-specialty medical center during quarantine. We were expected to open May 5, 2020, but had to halt construction during quarantine with no expected return date. Which meant we could not get patients on the schedule because we didn’t know when the building would be available for us to start, or even if quarantine would be lifted. So, we did a quick reframe and changed around our system and malpractice so we could open (even earlier than expected!) via telemedicine. Thankfully, we were able to do that for the 1st 2 1/2 months and then, at the end of June, we opened in person. What a relief! We did have to spend more money than budgeted on PPE and had many last-minute cancellations due to covid. But many would ask me how Covid had affected our business and I had no good answer for them as I had no baseline to compare. We opened at the height of the pandemic!
Appreciate you sharing that. What should we know about Women’s+ Health Collective?
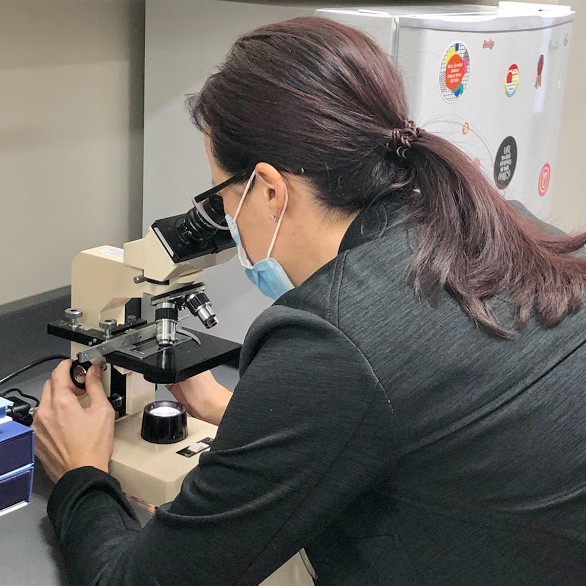
We are a Gynecologic practice incorporating sexual health, pelvic health, and mental health. We have certified and licensed experts available for our patients such as Certified Sex Counselors, Sex Educators, Board Certified Gynecologist, pelvic health Physical Therapist, Certified Sex Therapists, PAs with specialty training in psychiatry, sexual medicine, vulvar pain, vulvar skin disorders, and pelvic health, therapeutic and somatic bodyworkers, Reiki Master, Registered Dietitian, and a personal trainer. We are a practice that sees a high number of people who have experienced either medical, domestic, interpersonal violence, or trauma and who have high anxiety or avoidance of typical Gynecology practices. We also see patients with sexual health concerns of all types, with many expressing distress over low libido or sexual pain.
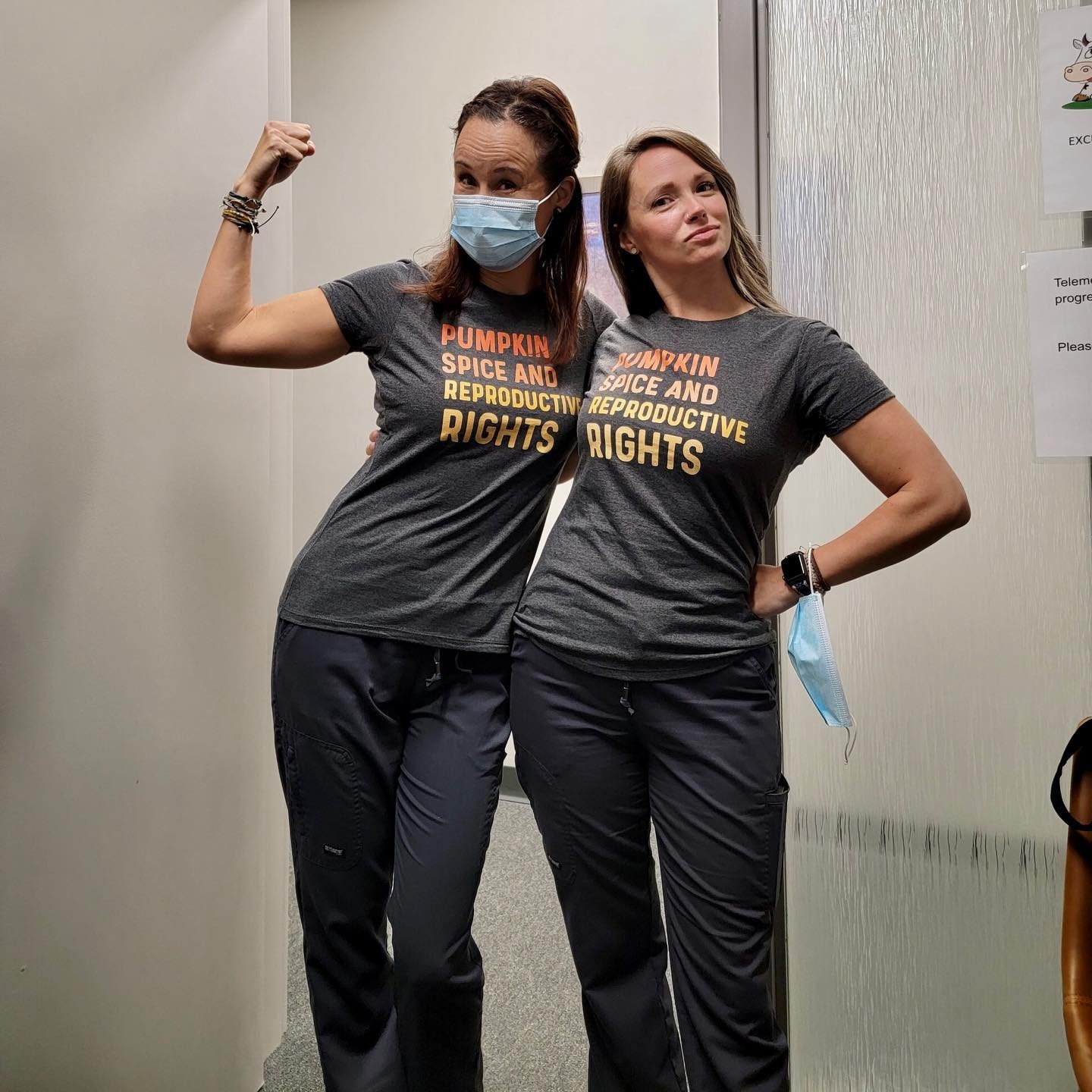
As a practice, we are very proud to provide a safe, non-judgmental and inclusive environment while also providing the most up-to-date and evidence-based care. We work daily to use “small” signs that show we are a safe space, such as affirming pins and earrings, signs that are supportive for those who are survivors of violence, T-shirts that de-stigmatize mental health, pride flags, no white coats worn by providers that might further amplify any perceived power differential, asking each patient if they would like to be weighed with signs by the scales of encouragement and highlighting the fact that weight does not equal health, and room setups that take into account privacy as well as the ability to keep the provider at the same physical level as the patient vs standing over the patient while they sit.
We also work to continually support and interact with our community. One way we accomplish this is by working with local artists in the BIPOC community and allowing them a free space to display their artwork. It’s been so beautiful to see each artist rotate through gracing our space with their amazing work.
Our providers are consistently involved in both educating the next generation of health care providers as well as continuing their own education. We are often known to give lectures both in our community as well as nationally to teach others how to implement healthcare in this way.
If we knew you growing up, how would we have described you?
I was a quiet, shy Asian American girl growing up in a typical Asian American household. I knew to stay quiet; I knew not to talk back or out of turn. I’ve said often I was scared of my own shadow, and that’s not far from the truth. My only interest was doing what my parents asked of me and hoping they would be proud of me. Therefore, I was good in school and an intense studier. I loved reading and babysitting – said another way, I loved what I love now, learning and taking care of people.
Contact Info:
- Email: [email protected]
- Website: https://www.whcollective.com/
- Instagram: https://www.instagram.com/whcollective/?hl=en
- Facebook: https://www.facebook.com/nishamckenziePA
- Youtube: https://www.youtube.com/channel/UC6M8czHKTzPzBd3OlstflEA
- Yelp: https://www.yelp.com/biz/womens-health-collective-grand-rapids
- Other: https://vm.tiktok.com/TTPdC4MNH5/